Hormonal vs. Copper IUDs: An In-depth Comparison
Introduction
Whether you are a healthcare provider guiding patients through their contraceptive options or someone exploring methods for personal use, the choice between hormonal and copper IUDs is pivotal. Each type offers unique benefits and operates differently within the body. This article is a comparison to clarify the differences, helping doctors advise their patients effectively and enabling individuals to make well-informed decisions about their reproductive health.
What are Hormonal IUDs?
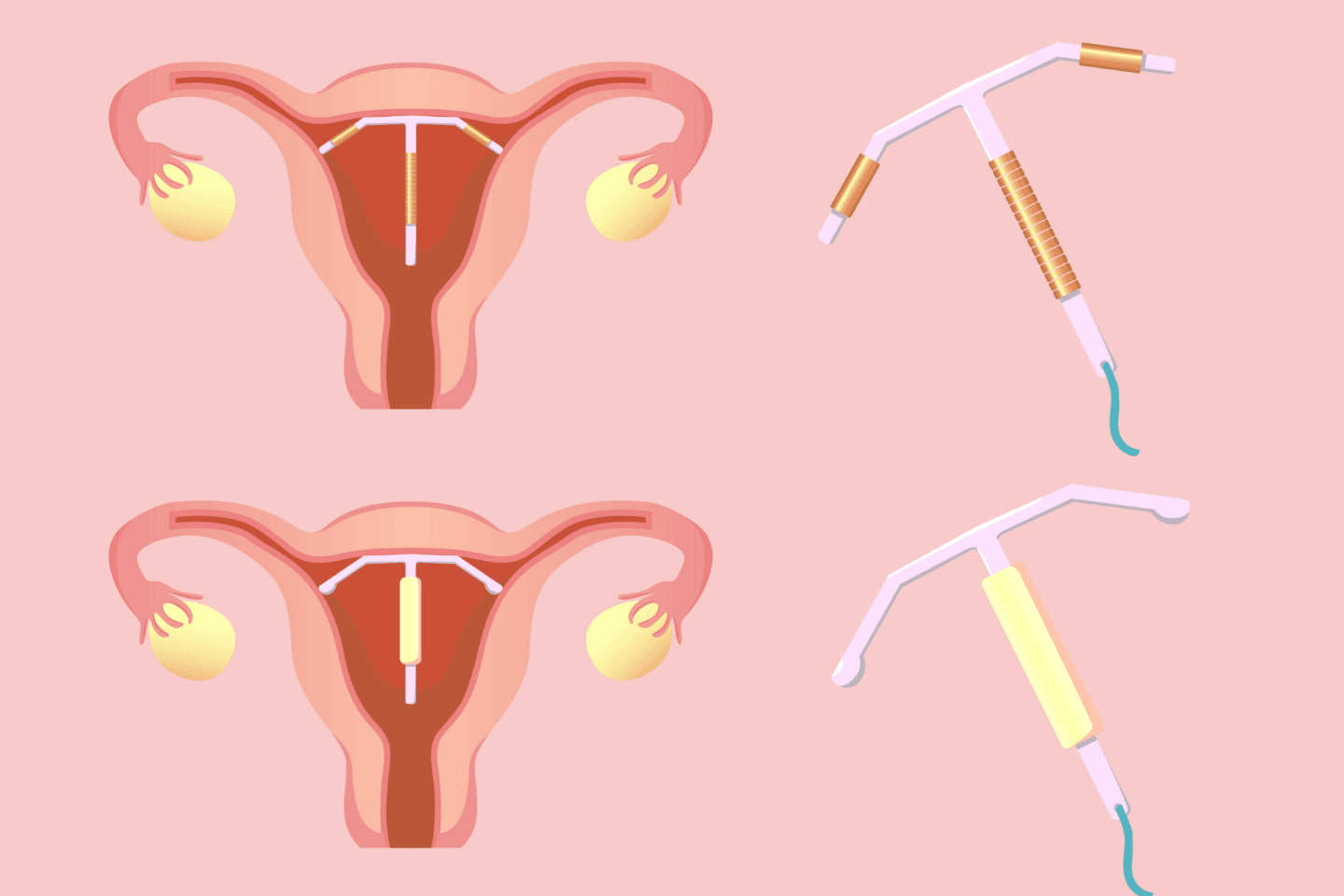
Hormonal IUDs are small, T-shaped devices inserted into the uterus, where they release a low level of progestin hormone. This hormone thickens the cervical mucus to prevent sperm from reaching an egg and thins the uterine lining, reducing the likelihood of implantation.
Advantages of Hormonal IUDs
Hormonal IUDs offer a range of benefits that cater to those seeking a reliable, long-term contraceptive solution.
- Longevity: Hormonal IUDs are designed for long-term use, offering continuous contraception for 3 to 6 years, depending on the specific product. This extended duration is ideal for individuals looking for a more permanent solution to birth control without the need for frequent replacements.
- Efficacy: With a success rate of over 99%[2], hormonal IUDs are among the most effective forms of contraception available today. This high level of efficacy is due to the constant release of hormones, which effectively prevents ovulation and creates a hostile environment for sperm in the uterus and fallopian tubes.
- Menstrual Benefits: Many users of hormonal IUDs experience significant menstrual benefits. The progestin hormone released by the IUD not only helps in contraception but also thins the lining of the uterus. This often results in lighter menstrual bleeding and fewer menstrual cramps, which can be a relief for those who previously suffered from heavy or painful periods.
- Reversible: One of the appealing features of hormonal IUDs is their reversibility. Fertility is typically restored quickly after the removal of the IUD, often within a month.
- Maintenance-Free: Once inserted, hormonal IUDs require no daily maintenance, making them a convenient choice for those with busy lifestyles or those who prefer not to manage daily pills. The user can essentially 'set and forget' this form of contraception for several years. Routine checks are minimal, generally involving an initial check-up after insertion and periodic follow-ups to ensure everything remains in place and functions as intended.
Understanding Copper IUDs
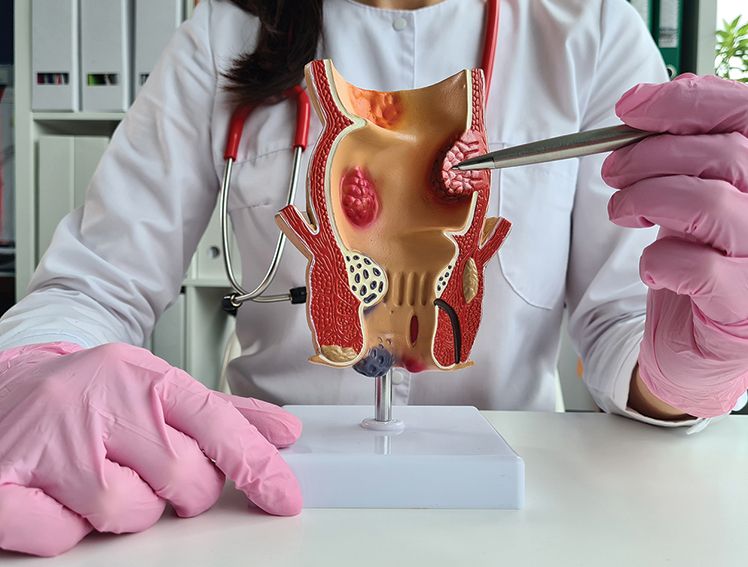
Copper IUDs, also T-shaped and placed within the uterus, work by releasing toxic copper ions to sperm, thereby preventing fertilisation. Unlike their hormonal counterparts, copper IUDs do not contain any hormones.
Advantages of Copper IUDs
Copper IUDs stand out as a reliable and hormone-free option for long-term contraception. Below are the detailed advantages of choosing a copper IUD:
- Duration: One of the most significant advantages of the copper IUD is its duration of effectiveness—it can provide contraception for up to 10 years. The copper IUD's longevity offers convenience and makes it a cost-effective solution over the years, eliminating the need for frequent replacements or routine medical interventions.
- Non-Hormonal: Copper IUDs do not contain hormones, making them an excellent option for those who prefer to avoid hormonal contraceptive methods. The copper IUD offers effective contraception without the systemic effects that hormones can have on the body.
- Immediate Effectiveness: Copper IUDs start working immediately after insertion. This immediate onset of action ensures that protection against pregnancy begins right from the time of placement, providing peace of mind without the need for backup contraception.
- High Efficacy: Copper IUDs are more than 99% effective at preventing pregnancy. This high level of protection is maintained throughout the duration of use, regardless of natural fluctuations in hormones or changes in sexual activity.
Side Effects and Considerations of Hormonal and Copper IUDs
While IUDs are generally safe and effective for most women, like any medical device, they come with potential side effects and considerations. Understanding these can help individuals make informed choices and anticipate what to expect.
Hormonal IUDs
- Spotting Between Periods: Especially common in the first few months after insertion, users may experience irregular bleeding or light spotting.
- Hormonal Side Effects: Some individuals might notice hormonal changes such as mood swings, acne, headaches, or breast tenderness, particularly in the initial stages after insertion.
- Changes in Menstrual Patterns: Many users report reduced menstrual flow over time, but the initial months may include irregular or unpredictable bleeding patterns.
Copper IUDs:
- Heavier Menstrual Bleeding and Cramping: One of the most reported side effects of copper IUDs is an increase in menstrual bleeding and more pronounced cramps, particularly in the first few months after insertion.
- Menstrual Distress: Some users might experience significant menstrual pain and heavy bleeding, which, although often improving over time, can be challenging for some to manage.
Procedure and Maintenance of Hormonal and Copper IUDs
Both hormonal and copper IUDs follow a similar procedure for insertion and require comparable maintenance routines. However, being well-informed about each step can significantly enhance comfort and effectiveness.
Detailed Procedure Overview
- Consultation and Screening: Before the IUD insertion, a thorough medical screening is conducted to assess suitability for an IUD. This includes discussing medical history, current health conditions, and potential risks.
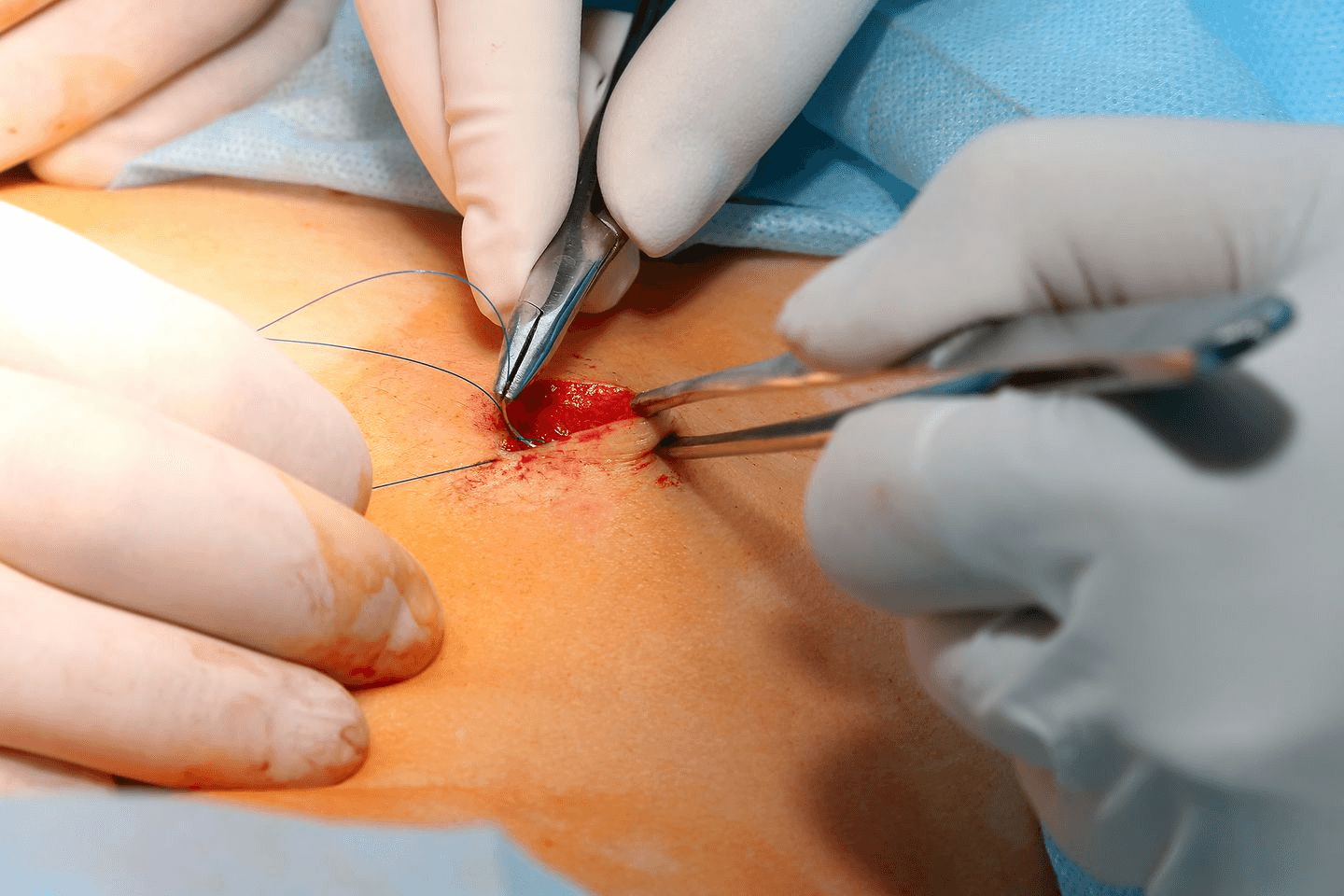
Pain Management: Some clinics may offer options to manage discomfort during the procedure. This might include local anesthesia or a cervical block to reduce pain sensations during the insertion. - Insertion Technique: Using sterile equipment, the healthcare provider gently inserts the IUD through the cervical canal into the uterus. The process is generally quick, but precision is crucial to avoid complications like perforation or improper placement. Once in place, the arms of the T-shaped IUD unfold to secure the device.
- Immediate Post-Insertion Care: After the IUD is in place, patients might stay under observation for a short period to manage immediate reactions like dizziness or cramping. Providers might also use an ultrasound post-insertion to confirm that the IUD is correctly positioned within the uterus.
Maintenance and Follow-Up Care
- Short-Term Follow-Up: The initial weeks after insertion are critical for ensuring the IUD remains properly positioned and the patient adjusts well. Any intense pain, excessive bleeding, or unusual symptoms should prompt an immediate consultation.
- Long-Term Care: Maintaining an IUD involves minimal effort beyond the first few months. Annual check-ups are recommended to ensure the IUD hasn’t shifted and to discuss any concerns. During these visits, the healthcare provider may perform a pelvic exam or an ultrasound to check the IUD’s placement.
- Self-Maintenance: Educating patients on how to feel for the IUD strings and recognising signs of potential issues is crucial. Patients should know how their strings typically feel and check them regularly to ensure the IUD has not moved. Changes in the length of the strings or the inability to feel them could indicate displacement or expulsion.
Managing Common Concerns
- Expulsion: Patients should be informed about the signs of expulsion, such as feeling the IUD itself at the cervix or outside the cervix. If suspected, they should contact their healthcare provider and avoid unprotected intercourse.
- Infections: It is essential to recognise the signs of potential infections early on. Symptoms such as fever, severe pelvic pain, or changes in discharge should be addressed immediately to prevent complications.
Removal and Post-removal Expectations of Hormonal and Copper IUDs
Removing an IUD is a straightforward procedure that healthcare providers can typically perform quickly and with minimal discomfort. Understanding what to expect during and after the removal can help manage any concerns and prepare for the transition, whether it involves switching contraceptives or planning for pregnancy.
Removal Process
- Scheduled Procedure: IUD removal is usually planned and often conducted at the end of its effective lifespan. However, it can be removed at any time upon a patient's request or for health reasons.
- Simple and Quick: During the removal, a healthcare provider gently pulls on the strings of the IUD with a specialised instrument. This action collapses the arms of the T-shaped IUD, allowing for its smooth exit through the cervical canal.
- Immediate Recovery: The removal process is typically painless for most, though some may experience mild cramping or spotting. Patients are usually able to resume normal activities immediately after the procedure.
Post-removal Expectations
- Return to Fertility: One of the significant benefits of both hormonal and copper IUDs is the rapid return to fertility. Most women find that their fertility returns to pre-IUD levels quickly, often within the first month after removal. This makes IUDs an excellent option for those considering future pregnancies.
- Menstrual Cycle Normalisation: After a hormonal IUD is removed, menstrual periods may return to the pre-IUD pattern. For copper IUD users, any increase in menstrual flow or cramping typically experienced during use should gradually decrease.
- Monitoring for Abnormal Symptoms: Post-removal, it's crucial to monitor for any abnormal symptoms such as severe pain, excessive bleeding, or signs of infection. While rare, complications can arise, and prompt medical attention may be necessary.
Additional Factors to Consider When Choosing Between Hormonal and Copper IUDs
Choosing between a hormonal and copper IUD involves considering several personal factors, such as:
- Immune System Conditions: For individuals with autoimmune disorders or immune system conditions, the choice between a hormonal or non-hormonal option like the copper IUD may be influenced by how hormones could potentially impact their immune response or disease status.
- Psychological Effects: Some people experience mood changes or other psychological effects from hormonal contraceptives. Those with pre-existing mental health conditions, such as anxiety or depression, might find that hormone-free options like the copper IUD better align with their health.
- Interaction with Other Medications: Hormonal IUDs can interact with other medications, potentially diminishing their contraceptive effectiveness or the effectiveness of other treatments. Those on long-term medication should consider this interaction when choosing an IUD type.
FIONA BY MERIL
Fiona is a hormonal intrauterine device (IUD) equipped with a drug reservoir containing levonorgestrel. Designed for simplicity and safety, it features a lock mechanism and offers up to five years of effective contraception. Key benefits of Fiona include reduced menstrual bleeding, prevention of endometrial issues, and no significant impact on body weight. Its cost-effectiveness and non-disruptive nature to sexual activities are also emphasized.
ERINNA BY MERIL
Erinna, hormonal IUD using levonorgestrel, provides effective contraception for up to five years. It is noted for its ease of use and ability to reduce menstrual bleeding while also potentially preventing endometrial complications. Like Fiona, Erinna minimally impacts sexual activity.
MERITE BY MERIL
MeriTe by Meril offers a range of intrauterine contraceptive devices (IUDs) designed to provide effective long-term contraception. The Merite Cu series, including Cu 375, Cu 250, and Cu 380 A, are copper-based IUDs known for their high efficacy and safety profiles. These devices are inserted into the uterus to prevent pregnancy by releasing copper ions, which are toxic to sperm. They are a popular choice for women seeking a non-hormonal, reversible contraceptive method that offers protection for several years.
Final Thoughts
Both hormonal and copper IUDs offer effective, long-term contraception but differ in their operation and side effects. Understanding these differences and consulting with healthcare providers will guide individuals in choosing the best intrauterine device for their reproductive health needs.
References
https://health.clevelandclinic.org/do-the-benefits-of-iuds-outweigh-the-potential-side-effects
https://www.webmd.com/sex/birth-control/types-of-iuds-which-one-is-right-for-you#:~:text=hormonal%20IUDs%20are%20successful%2099.8%25%20of%20the%20time
https://health.clevelandclinic.org/copper-birth-control
https://www.plannedparenthood.org/learn/birth-control/iud/iud-side-effects
https://my.clevelandclinic.org/health/treatments/24441-intrauterine-device-iud#procedure-details
https://www.webmd.com/sex/birth-control/iud-removal
https://my.clevelandclinic.org/health/treatments/24441-intrauterine-device-iud
https://www.nationwidechildrens.org/family-resources-education/health-wellness-and-safety-resources/helping-hands/birth-control-non-hormonal-iud#:~:text=The%20copper%20IUD%20is%20put,the%20IUD%20is%20in%20place.
https://www.plannedparenthood.org/learn/birth-control/iud/what-are-the-disadvantages-of-iuds
https://www.medicalnewstoday.com/articles/copper-iud
https://www.news-medical.net/health/IUD-Advantages-and-Disadvantages.aspx
https://www.betterhealth.vic.gov.au/health/healthyliving/contraception-intrauterine-devices-iud
https://www.medicalnewstoday.com/articles/323230
https://www.merillife.com/blog/innovations/iud-birth-control-a-boon-to-family-planning