Percutaneous Coronary Intervention- Restenosis & The Role of Bare Metal Stents and Drug Eluting Stents in Preventing It
Introduction
The role of different stents in treating coronary artery disease is under considerable discussion, emphasizing the superiority of clinical performance, improved outcomes, and long-term benefits of one type over the other. Stent placement is a percutaneous coronary intervention for treating blocked arteries, interrupting the smooth blood supply to the heart. Interventional cardiology has emerged over the years, from plain balloon angioplasty to using dissolving stents in PCI. This evolution has witnessed various generations of stents, each providing an improved version of the previous generation in terms of its clinical performance, reduction in potential risks and complications, vessel healing, and long-term safety and efficacy.
PCI faces complex adversities in highly calcified plaque, diffused diseased arteries (larger section of the artery is blocked with high plaque buildup), or arteries with soft and shaggy plaque, and the chances of restenosis post-stent placement. An optimum stent that caters to the clinical need to overcome all these adversities effectively is still to be defined. However, a relative study between stents helps us to understand the advantages of one over the other.
The blog discusses two such stents, the bare metal and drug-eluting stents, each having contributed considerably to treating CAD.
What is Stenosis?
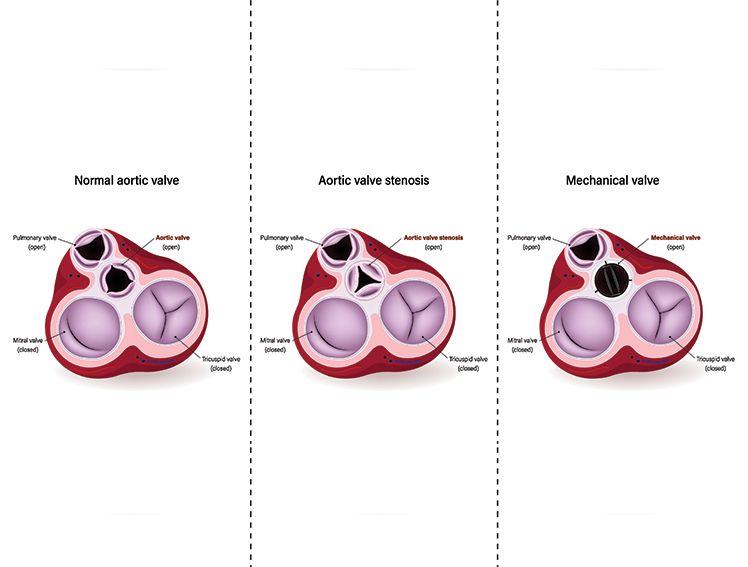
PCI treats coronary artery disease (CAD). CAD is caused by the narrowing of the coronary arteries (supplying oxygenated blood to the heart) due to plaque accumulation over time. The narrowing of the arteries is called stenosis. The condition of the plaque buildup is known as atherosclerosis. Plaque, a fatty substance, is medically known as atheroma.
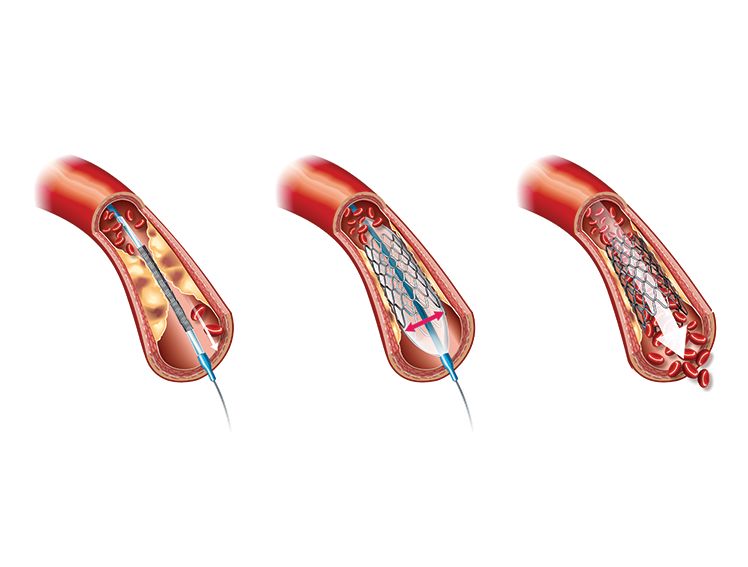
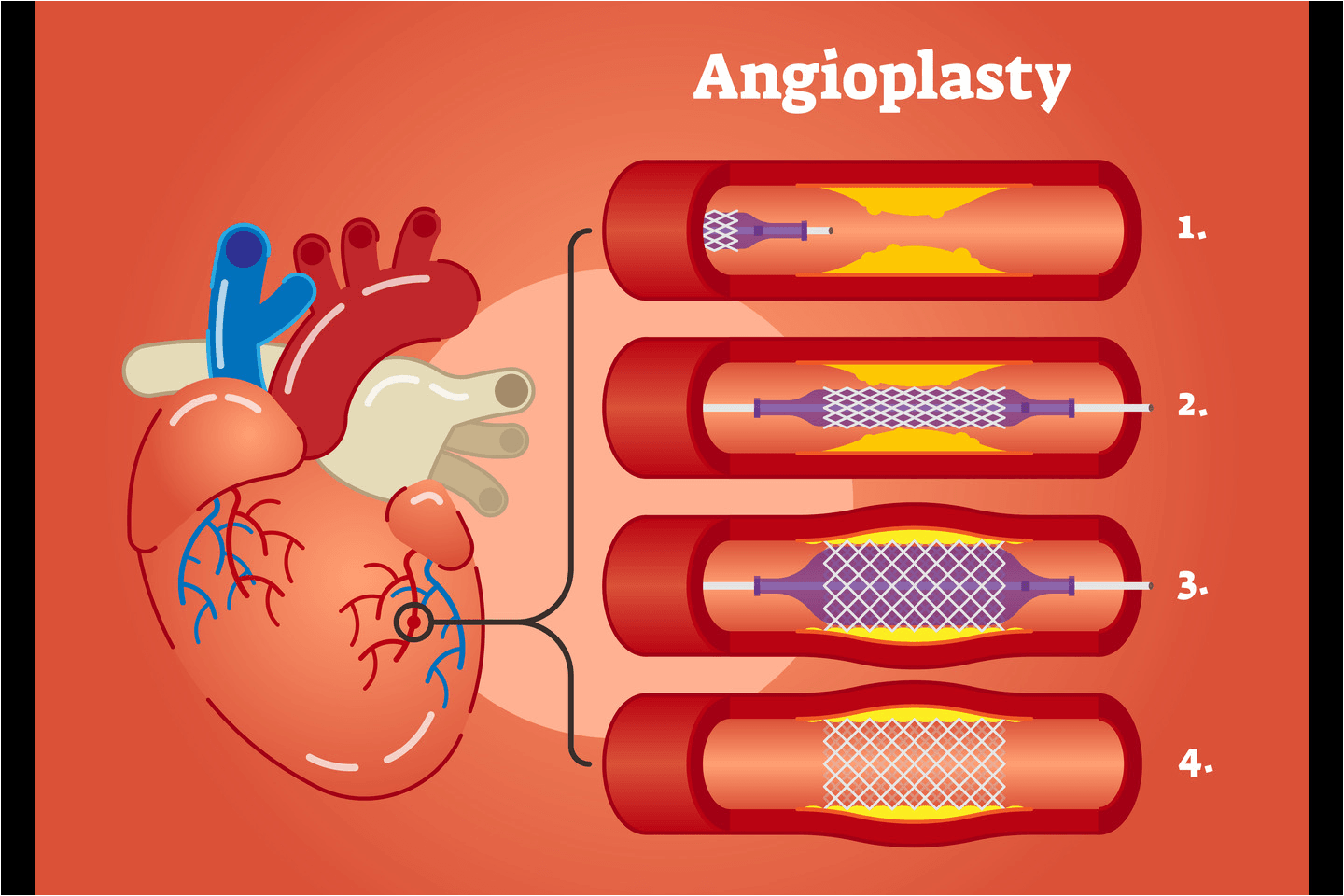
A stent is a small mesh-like tube placed in the arteries, using a catheter to keep them open for the oxygenated blood to flow uninterruptedly to the heart muscle. It is placed in the treated artery after the plaque is pushed to the arterial walls by inflating a balloon, sitting on the tip of the catheter, and reaching the plaque site. The percutaneous procedure of opening the blocked artery is known as angioplasty.
What is restenosis?
Angioplasty with a stent carries the risk of re-narrowing of the treated artery due to in-stent restenosis. The growth of tissue around the stents keeps them in place. The new lining of the arterial wall formed with the tissue growth helps in the smooth flow of the blood. However, when scar tissue grows underneath the lining, it thickens the arterial wall, causing the re-narrowing of the passage of the artery. This is known as restenosis. The contributing factors to restenosis are high cholesterol, high sugar levels, smoking, high blood pressure, or kidney disease.
Restenosis is thus the recurrence of stenosis in the treated artery. It usually occurs within the period of one to six months after PCI. Restenosis is the result of –
- Neointimal hyperplasia- caused by the proliferation and migration of vascular smooth muscle cells that thicken the arterial wall. The production of extracellular matrix that scaffolds the tissue and organs throughout the body is also the cause of restenosis.
- Thrombus formation- the formation of blood clots inside blood vessels.
- Elastic recoil- the inherent tendency of the tissue to resist change in shape and revert to the original shape after inflation.
Role of Bare Metal Stents (BMS) and Drug-Eluting Stents (DES) in PCI
Percutaneous Coronary Intervention revolutionized the treatment of CAD by relieving the obstruction in the arterial passage with minimal invasiveness, ensuring lesser pain, faster healing, and recovery. However, there were technical limitations and potential risks of frequent revascularisation, dissections, abrupt vessel closure, and elastic recoil. The efficacy and safety of PCI were challenged, and the need for improved alternatives that ensured short and long-term procedural safety and efficacy and positive patient care and outcomes arose. Introducing BMS and subsequent DES paved the way for advanced, improved, and preferred CAD treatment modes through PCI.
Bare Metal Stents (BMS)
A BMS is a thin metal stent, a mesh-like tube, used as a permanent scaffolding in the artery. It is an uncoated wire stent that keeps the artery open for the smooth flow of blood through the arterial passage once the plaque is pushed to the walls.
The first device was a stainless steel stent, with the current being made of cobalt chromium or platinum chromium.
As stated, Balloon angioplasty had its limitations. The introduction of BMS enabled PCI to become part of mainstream practice for treating CAD. BMS successfully overcame the limitations of Balloon angioplasty to a certain extent. The stent prevented abrupt vessel closure and elastic recoil, which was the major concern experienced with balloon angioplasty. However, the question of restenosis was still unresolved with the use of BMS. The device design and biocompatibility were the limiting factors of BMS. However, with advancement and improvement in the strut thickness of the stent, there were results of improved clinical performance and reduced in-stent restenosis post-PCI.
Drug-Eluting Stents (DES)
The role of Drug Eluting Stent, a milestone in interventional cardiology, is demonstrated by its use in treating CAD effectively, catering to the limitations of the BMS, primarily in preventing stent restenosis. The DES was initially introduced with anti-proliferative drug coating on standard BMS. The subsequent generations of DES and their improvised anti-proliferative drug compositions led to PCI entering the mainstream practice of CAD and the preferred choice of stent placement.
In subsequent generations, DES succeeded in overcoming the limitations of its earlier generation types with technological improvements, thinner strut stent thickness, improved anti-proliferative drug coatings, and new polymer usage. Each improved DES led to increased biocompatibility, thus taking care of its previous deficiencies. DES has clinically proved to be superior to BMS in preventing in-stent restenosis. They have contributed to reducing neointimal proliferation, one of the main causes of in-stent restenosis. These stents have also reduced the need for repeat revascularizations in CAD patients. However, the concerns of stent thrombosis and complications associated with dual antiplatelet therapy post-PCI, though addressed considerably, are not ruled out with the use of DES.
It would not be out of place to mention that despite the popularity and acceptance of DES over BMS, the latter still plays a vital role in treating CAD. BMS is preferred over DES for the reasons below:
- The damage to the endothelial layer (the layer formed by endothelial cells that lines the blood vessels and regulates exchanges between the bloodstream and tissues) is more by DES than BMS.
- There is a high risk of bleeding associated with the need for dual antiplatelet therapy after DES.
- The affordability of the DES becomes a concern for patients.
- The risk of restenosis perceived is low in large coronary vessels.
FROM MERIL BIOMIME™
BioMime™ is a Sirolimus-Eluting Coronary Stent System with an ultra-thin (65 µm) strut thickness. This next generation (SES) has a Novel Hybrid Design with closed cells, allowing for Morphology Mediated Expansion for adequate conformability and lesser edge dissections. Stent design with non-linear S links & Y connectors allowing high flexibility and adequate side branch access. Strut width variability ensures optimal radial strength.
EVERMINE50
EVERMINE50 is a breakthrough in DES Technology with its-
- Ultra-low strut thickness of 50μm for promoting early vascular healing.
- Variable strut width and variable crown design to ensure adequate radial strength.
- Hybrid cell stent design for optimal scaffolding and conformability.
- Clinically established drug Everolimus with biodegradable polymer for proven clinical safety & long-term efficacy.
Conclusion
Over the years, PCI has emerged as a preferred choice of revascularization and a safer and more efficacious treatment modality for CAD. The introduction of various stents with improvisations has brought drastic clinical solutions in terms of preventing elastic recoil, abrupt vessel damage, improved delivery, biocompatibility, and reduction in incidences of restenosis, stent thrombosis, risks associated with dual antiplatelet therapy, to mention a few.
The use of stent type is the decision of the interventional cardiologist arrived at after considering various factors, such as the age and anatomy of the patient, the severity of the condition, comorbidities, if any, the potential associated risks with the stent use, and the preference of the patients.
References
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5759296/#:~:text=Background,respect%20to%20their%20mechanical%20performance.
https://www.nejm.org/doi/full/10.1056/nejmoa1607991
https://www.acc.org/Latest-in-Cardiology/Articles/2016/10/20/10/47/There-Are-No-Current-Indications-to-Use
https://www.sciencedirect.com/topics/nursing-and-health-professions/bare-metal-stent#:~:text=Bare%20Metal%20Stents&text=Stainless%20steel%20BMSs%20were%20the,target%20lesion%20revascularization%20(TLR)