Medical Devices
Common Questions About Drug Eluting Stents, Answered
Heart problems can be daunting, leaving many patients and their families searching for answers. If you or someone you know has been advised to undergo angioplasty, you might have heard about "stents" or, more specifically, "drug-eluting stents." But what exactly are these? Why are they often recommended by doctors, and what makes them different from other types of stents? Understanding these details can make a huge difference.
What are Drug-Eluting Stents?[1]
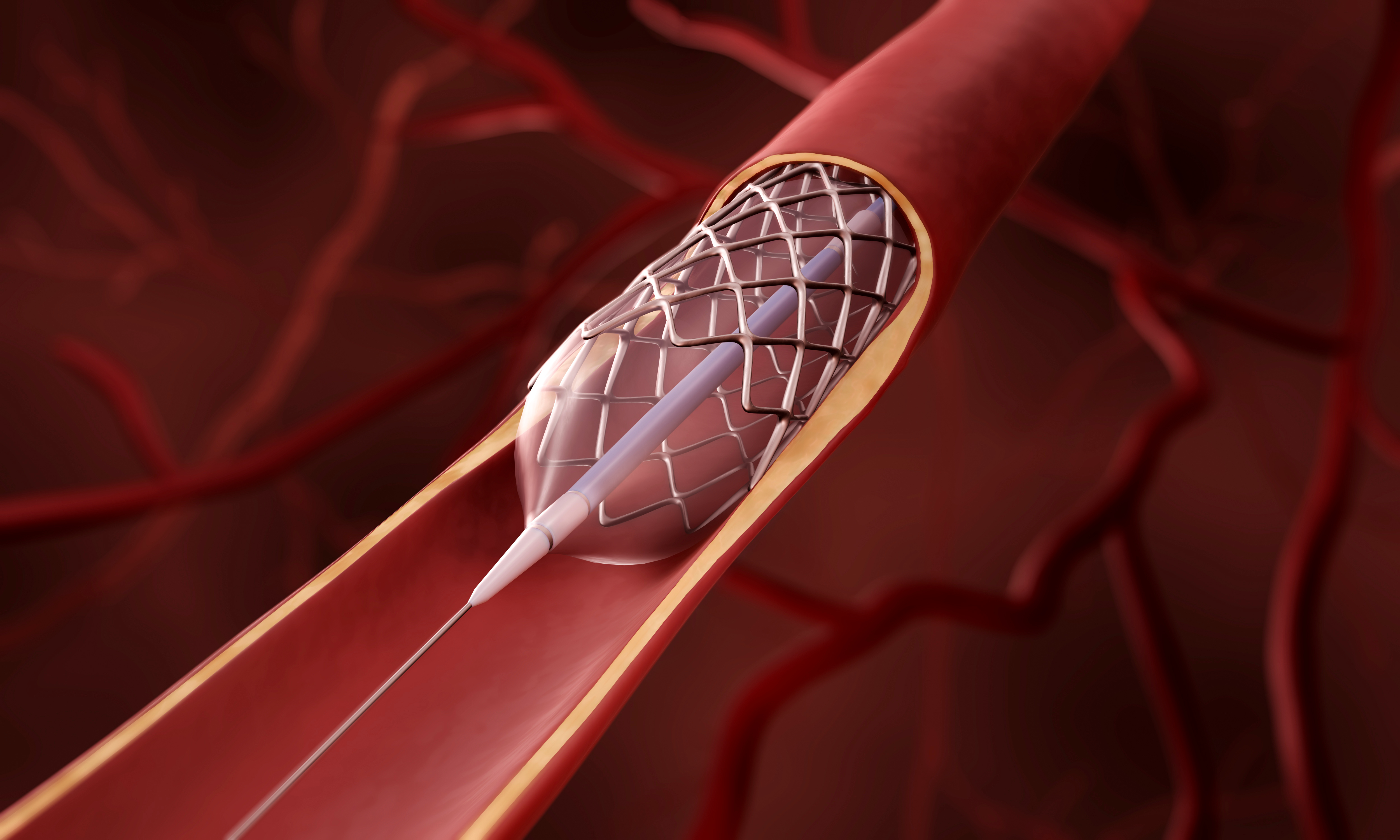
A stent is a tiny, mesh-like tube that is inserted into a blocked artery to help keep it open, allowing blood to flow freely. Stents are often used in a procedure called angioplasty, where blocked or narrowed arteries are widened. A drug-eluting stent (DES) is a type of stent coated with medication that is slowly released into the artery to prevent it from narrowing again. Unlike bare-metal stents, which do not have any coating, drug-eluting stents offer the added advantage of reducing the risk of restenosis or the re-narrowing of the artery.
Common Questions About Drug-Eluting Stents
Understanding drug-eluting stents involves knowing how they work, their benefits, and who they are suitable for. Here, we answer some of the most frequently asked questions.
1. How Do Drug-Eluting Stents Work?[1]
Drug-eluting stents work by releasing a drug over a period of time after the stent is implanted. The stent holds the artery open, and its drug coating helps stop scar tissue from narrowing again (restenosis). The medication is usually an anti-proliferative agent that prevents the cells in the artery wall from multiplying rapidly. This helps in keeping the artery open for a longer time and reduces the need for repeat procedures.
2. What are the Benefits of Drug-Eluting Stents?[1]
The primary benefit of drug-eluting stents is their ability to significantly reduce the risk of restenosis. This reduces the likelihood of needing another angioplasty or surgery in the future. Other benefits include improved blood flow, less angina or chest pain, and a quicker return to normal activities. Drug-eluting stents also help improve the overall quality of life of patients suffering from coronary artery disease.
3. What is the Procedure for Implanting a Drug-Eluting Stent?[1]
The drug-eluting stent is implanted via a procedure called angioplasty, a minimally invasive procedure. It involves inserting a small balloon catheter into a blood vessel. This is usually in the groin or wrist and guides it to the blocked coronary artery. Once that is in place, the balloon is inflated to open the artery, and a drug-eluting stent is deployed. The stent expands and locks in place, providing support to the artery walls. Then, the balloon is deflated and removed, allowing the stent to remain in place and keep the artery open. The procedure usually takes about one to two hours, and most patients can go home within a day or two.
4. Who is Eligible for Drug-Eluting Stents?[1]
While drug-eluting stents are effective, they are not suitable for everyone. They are generally recommended for patients with coronary artery disease who have at least one narrowed artery that is suitable for stenting. However, individuals who cannot take long-term blood-thinning medications may not be good candidates for drug-eluting stents. A cardiologist will evaluate the patient's condition, medical history, and specific needs before recommending the most suitable type of stent.
5. How Long Do Drug-Eluting Stents Last?[1]
Drug-eluting stents are designed to be permanent. They remain in the artery for life to provide ongoing support and prevent re-narrowing. The drug coating on the stent is gradually released over a period of months, after which only the metal framework remains. While drug-eluting stents greatly reduce the risk of restenosis, they are not a cure for coronary artery disease. Patients must continue to follow a heart-healthy lifestyle, take prescribed medications, and attend regular follow-ups with their doctors to ensure the stent remains effective.
Biomime by Meril
Biomime by Meril is an advanced drug-eluting stent system designed for the effective treatment of coronary artery disease. Biomime combines an ultra-thin strut design with a biodegradable polymer that releases sirolimus, minimizing restenosis and enhancing vascular healing. Its unique Hybrid Cell Design ensures optimal flexibility, conformability, and radial strength, making it suitable for challenging and complex lesions. Biomime is crafted to offer superior clinical outcomes, ensuring long-term safety and efficacy for patients undergoing angioplasty.
Conclusion
Deciding on the right treatment for heart conditions can be overwhelming, but being well-informed about your options is a crucial step toward better health. Remember, the journey to a healthier heart does not end with a stent—it involves a commitment to a healthy lifestyle and regular follow-ups. Act now, educate yourself and take charge of your heart health today.
Reference Links:
[1] https://www.webmd.com/heart-disease/what-to-know-about-drug-eluting-stents
[2] https://www.ahajournals.org/doi/full/10.1161/CIRCULATIONAHA.107.688176